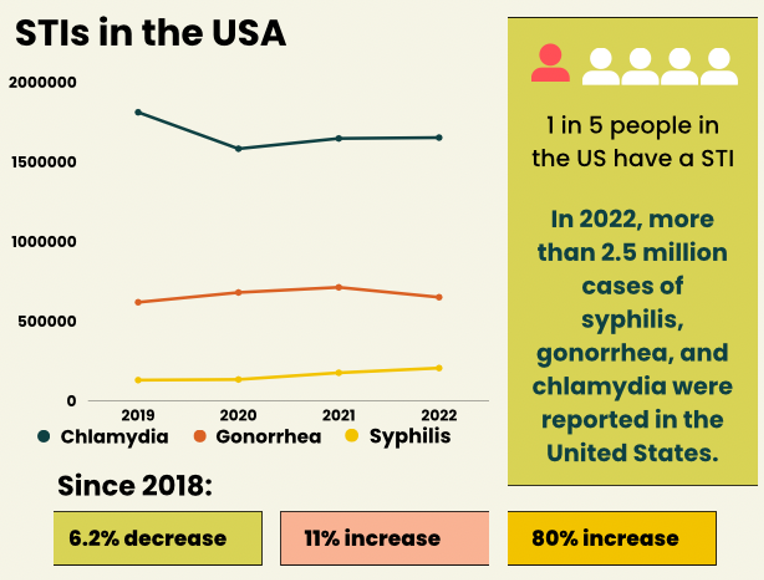
Each year approximately 2.5 million cases of sexually transmitted infections (STIs) are reported in the United States. In recognition of the recent observance of STI Awareness Week, Keystone Infectious Disease’s Medical Director, Dr. Raghavendra Tirupathi, and medical students studying under him, Ananya Prakash, Aasim Akthar and Shashvat Joshi, answer common questions about STIs in today’s article.
What are STIs and who is most commonly affected?
STIs pose a significant public health challenge globally, affecting individuals of all ages and demographics. The Centers for Disease Control and Prevention (CDC) defines STIs as infections that are spread by sexual contact.
Young individuals, aged 15-24, bear a disproportionate burden of STIs. This age group accounts for half of all new STI diagnoses, primarily due to risky behavior, limited healthcare access, inadequate education and stigma surrounding testing, leading to higher transmission rates.
 What are the symptoms?
What are the symptoms? There are several types of STIs, with the most common including chlamydia, gonorrhea, syphilis, herpes simplex virus type 2, trichomoniasis and human papillomavirus (HPV).
Chlamydia and gonorrhea can be hard to diagnose as they often show no symptoms at first, but can later lead to painful or burning urination, abnormal discharge from the penis or vagina, abdominal pain and painful intercourse. If left untreated, they can cause serious complications, including infertility.
Syphilis progresses through stages: painless genital sore(s) in the primary stage, followed by a rash, fever and fatigue in the secondary stage. If untreated, it can enter a latent stage with no symptoms and progress to severe complications affecting multiple organs.
Genital herpes often causes painful blisters or sores in the genital region that can itch or burn. These sores can open up and become ulcers before eventually healing. Additionally, some individuals may have flu-like symptoms like fever and swollen glands during outbreaks.
Trichomoniasis symptoms include greenish-yellowish vaginal discharge, genital itching and irritation and pain and discomfort during urination or intercourse.
HPV is the most common sexually transmitted infection in the USA and includes several types. The lower-risk types, HPV 6 and 11, are known to cause small flesh-colored genital warts, while HPV 16, 18, 31 and 33 can cause cervical, anal, head and neck cancer.
How can I stay safe?
Taking proactive steps in sexual wellness is crucial for overall health. Consistently using barrier contraceptives, like condoms, and undergoing regular STI testing, especially for sexually active individuals or those with multiple partners, are important practices. Early screening allows for timely treatment, reducing complications. Open communication with partners about testing and prevention strategies builds trust and empowers informed decisions. Assessing individual risk factors and adopting preventive measures, such as limiting your number of sexual partners and avoiding high-risk behaviors, further minimizes STI transmission.
Regular testing is also very important. Testing is available for little or no cost through the Department of Health or at Federally Qualified Health Centers like Keystone. Given that many STIs don’t show symptoms at first, routine testing helps with early detection, treatment and prevention of complications.
What tests are available?
There are various types of tests including urine samples, swab tests and blood tests. Tests performed at healthcare facilities are highly accurate and some even have results in 20 minutes.
Self-test kits are also an option for some STIs like HIV and syphilis. These kits empower individuals to test in the privacy of their own home, making it convenient for those who may face barriers to traditional healthcare or live in areas with limited resources. Some kits only test for one particular STI, so it’s important to read the label carefully.
Who should get tested?
The CDC recommends all individuals aged 13-64 get tested for HIV at least once. Annual testing is advised for anyone engaging in behaviors that may heighten their risk of HIV infection.
For women, routine screening for gonorrhea and chlamydia is important for those who are sexually active, especially women under 25, with additional testing recommended for women 25 and older who have specific risk factors such as multiple sexual partners. Pregnant women should have a full STI screening early in the pregnancy, testing for syphilis, HIV, hepatitis B and hepatitis C, with chlamydia and gonorrhea screening advised for those at risk. Repeat testing may be necessary for some patients.
Men who have sex with men (MSM) face unique challenges in sexual health. The CDC recommends annual screening for syphilis, chlamydia, gonorrhea and HIV, with increased testing frequency for those with multiple or anonymous partners. Additionally, annual hepatitis C screening is recommended for MSM living with HIV.
How are STIs treated?
STIs are typically treated with antibiotics or antiviral medications. It’s important to complete the full course of treatment as prescribed by a healthcare provider, even if symptoms improve before the medication is finished. Regular testing and treatment of sexual partners may also be necessary to prevent reinfection and spread. Effective STI treatments are crucial for both individual and public health.
In the ongoing battle against STIs, innovative approaches are emerging to enhance prevention efforts. From groundbreaking educational campaigns to the development of accessible testing kits, new strategies are reshaping how we approach sexual health. Pre-Exposure Prophylaxis (PrEP) represents a significant advancement in HIV prevention. Doxycycline prophylaxis shows promise in preventing STIs in MSM living with HIV who have a history of recurrent syphilis, with up to a 73% reduction in bacterial STI occurrence observed.
While most cases of STIs can be treated by a prescription, there is growing concern in the medical community about drug-resistant gonorrhea. Each year, over 500,000 cases of gonorrhea are reported, but the CDC estimates the actual number of new infections could be as high as 1.6 million. Alarmingly, approximately half of these infections show resistance to at least one antibiotic, highlighting the growing challenge of antibiotic-resistant gonorrhea, making it harder to treat. This resistance poses a significant public health threat, as it complicates efforts to control and manage the spread of the disease. This is yet another reason why practicing safer sex is so important.
What are some common misconceptions?
Dispelling prevalent misconceptions about STIs is important in reducing rates of infection. Some common myths include: only promiscuous individuals contract STIs and/or they are punishment for immoral behavior, infections always show symptoms and STIs can only be transmitted through penetrative intercourse (in reality, STIs can be spread through vaginal, anal and oral sexual contact).
Health workers play a vital role in this initiative by providing accurate information, delivering non-judgmental care and fostering open dialogues about sexual health. To combat these myths, society should cultivate an atmosphere of understanding and empathy, advocating for non-judgmental attitudes and encouraging proactive healthcare-seeking behaviors. Through the collaboration of health workers and community efforts, we can challenge stigma and establish a more informed and inclusive society.
 Summary
SummarySTIs are a public health concern affecting individuals worldwide, regardless of age or other demographics. They encompass a range of infections spread through sexual contact, including vaginal, anal and oral sex.
Symptoms vary depending on the specific infection but may include painful urination, abnormal discharge, genital sores or blisters, flu-like symptoms and itching. However, many STIs can show no symptoms for extended periods, underscoring the importance of regular testing.
Getting tested ensures early detection of STIs, allowing for necessary treatment to prevent complications and reduce the risk of transmission to others. Treatment for STIs often involves antibiotics for bacterial infections like chlamydia, gonorrhea and syphilis, while antiviral medications are used for viral infections such as genital herpes. Prompt diagnosis and following the treatment plan is essential to prevent complications and limit spread.
Prevention strategies include consistent and correct condom use, regular STI testing, limiting the number of sexual partners and open communication with sexual partners about testing and prevention. Vaccinations are also available for certain STIs like HPV and hepatitis B, offering additional protection.
In summary, raising awareness, undergoing routine testing and implementing proactive prevention strategies are essential in addressing the spread of STIs and fostering sexual well being. Through emphasizing education, reducing the stigma of testing and advocating for readily available healthcare services, individuals can take responsibility of their sexual health and play a role in building healthier communities.
This article contains general information only and should not be used as a substitute for professional diagnosis, treatment or care by a qualified health care provider.