Penicillin allergy is one of the most reported drug allergies in the U.S., but the vast majority of those reports are inaccurate. Understanding the truth behind this allergy is crucial—not just for your personal care, but for public health and antibiotic stewardship. Keystone Infectious Disease’s Medical Director, Dr. Raghavendra Tirupathi, and medical students studying under him, Jay Patel and Nandini Patel, explain what you should know.
Are Most Penicillin Allergies Real?
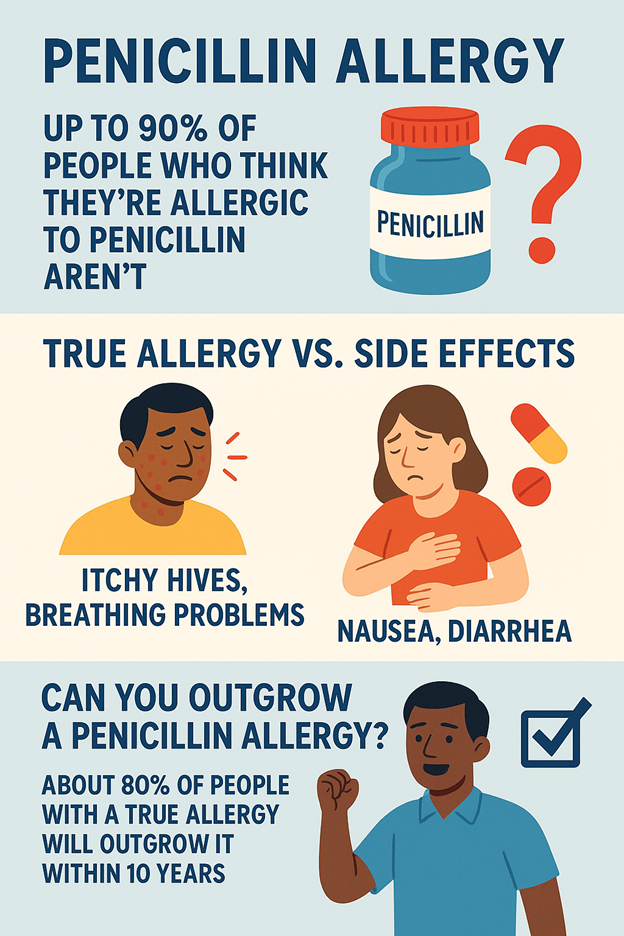
Not always. Up to 90% of people who think they’re allergic to penicillin actually aren’t. Many allergy labels are based on childhood reactions, vague symptoms or side effects—and never get updated.
What Is Penicillin?
Penicillin is one of the oldest and most commonly used antibiotics. It was discovered in 1928 and is used to treat many bacterial infections, including strep throat, ear infections, pneumonia and skin infections. It works by stopping bacteria from building their protective cell walls, essentially killing the infection at its source.
What Should You Know If You’ve Been Told You’re Allergic to Penicillin?
Many people are told they’re allergic to penicillin, but the details matter. It’s important to know what kind of reaction you had—was it a rash, nausea or something more serious like trouble breathing?
If you’ve had a severe reaction in the past (like swelling of the throat or difficulty breathing), wear a medical alert bracelet and make sure your doctors know. If your reaction was milder, like a rash or hives, write down the symptoms and the timeline. The more specific you are, the better your provider can assess whether it was a true allergy or something else. Side effects like nausea or diarrhea are not true allergies, but they often get recorded as one and stay in your medical history for years.
Was It a Side Effect or a True Allergy?
Side effects are common with many medications. These may include nausea, diarrhea and mild stomach discomfort. These symptoms usually happen after a few doses and are related to how your body digests the drug—not an immune reaction.
In contrast, a true penicillin allergy involves your immune system and typically shows up within minutes to an hour of taking the medication. These reactions can include itchy hives or welts, swelling of the lips, face or hands, breathing difficulty or chest tightness and feeling dizzy or faint due to low blood pressure.
If any of these occur, seek medical help immediately, as they may signal a life-threatening condition called anaphylaxis (a severe allergic reaction).
What Are the Symptoms of a Penicillin Allergy?
Mild symptoms may include an itchy rash or hives (red welts on the skin) and swelling of the face, lips, hands or feet. These symptoms are uncomfortable but usually go away with allergy medicines like antihistamines or steroids.
Severe symptoms (anaphylaxis) may include swelling of the tongue or throat, difficulty breathing, chest tightness and dizziness or fainting (caused by a drop in blood pressure). Call 911 right away if you experience these. Emergency treatment may include epinephrine and IV medications.
Can You Outgrow a Penicillin Allergy?
Yes, about 80% of people with a true penicillin allergy outgrow it within 10 years. But many still carry the “penicillin allergy” label in their medical records for life, even if they’re no longer allergic. That’s why it’s important to ask your healthcare provider about penicillin allergy testing—a safe and effective way to find out for sure.

If I Was Told I’m Allergic Years Ago, Should I Still See an Allergist?
Yes, and here’s why. Many allergy labels are based on outdated or unclear information. A simple evaluation by an allergist, often including skin testing, can confirm whether you’re still allergic or if you were misdiagnosed in the first place. Getting reevaluated is especially important before surgery or hospital admission, where antibiotic options matter most.
Does Amoxicillin Count as Penicillin? Do I Need Testing?
Yes, amoxicillin is part of the penicillin family. If you were told you’re allergic to amoxicillin, it’s still important to get tested. An allergist can help you determine whether it’s a true allergy or if it’s safe for you to take penicillin-based antibiotics again.
Is Penicillin Allergy Genetic? Should I Be Concerned If It Runs in My Family?
No, penicillin allergy is not inherited. Just because a parent, sibling or relative has it doesn’t mean you will. There’s no need to avoid penicillin solely based on family history. If you’ve never had a reaction yourself, it’s usually safe to take, unless a doctor says otherwise.
What Happens if a False Penicillin Allergy Isn’t Corrected?
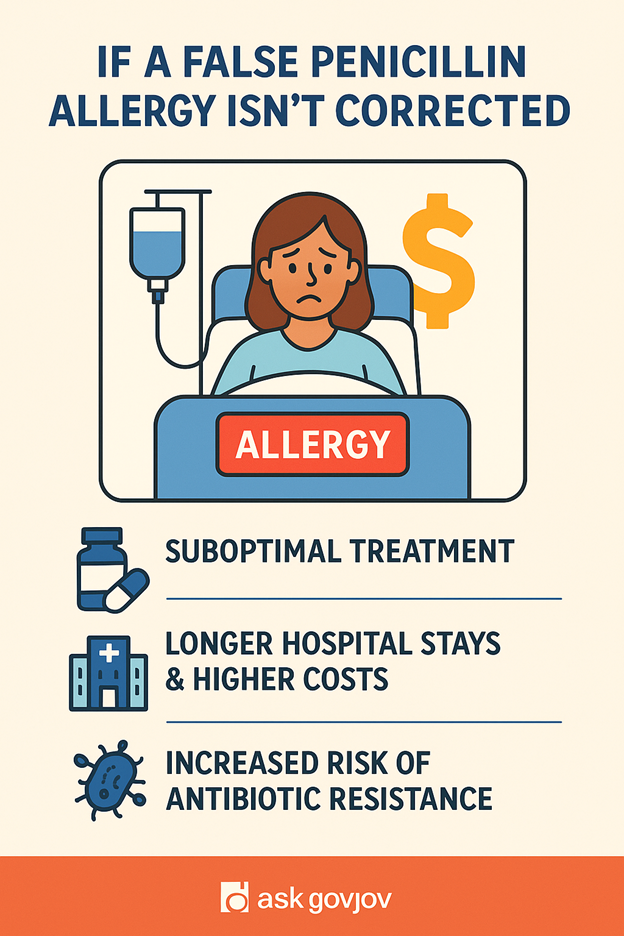
Leaving an unverified penicillin allergy unaddressed can have serious consequences. You may be prescribed broader-spectrum or second-line antibiotics that are less effective against certain infections, are more toxic and are associated with more adverse drug reactions. Your risk of infections can also increase as people with a penicillin allergy label are more likely to develop surgical site infections, drug-resistant bacterial infections due to the overuse of alternative antibiotics and Clostridioides difficile infections which is a severe, potentially life-threatening diarrheal illness.
Studies have shown that patients with a penicillin allergy label have longer hospital stays, incur higher healthcare costs and receive more unnecessary broad-spectrum antibiotics, contributing to antibiotic resistance. Using alternative antibiotics unnecessarily contributes to the rise of multi-drug resistant bacteria, a major global health threat. Infections like strep throat, syphilis and certain forms of pneumonia respond best to penicillin-based therapy. A false allergy can mean missing the safest and most effective treatment.
What Can You Do If You Have a Penicillin Allergy Label?
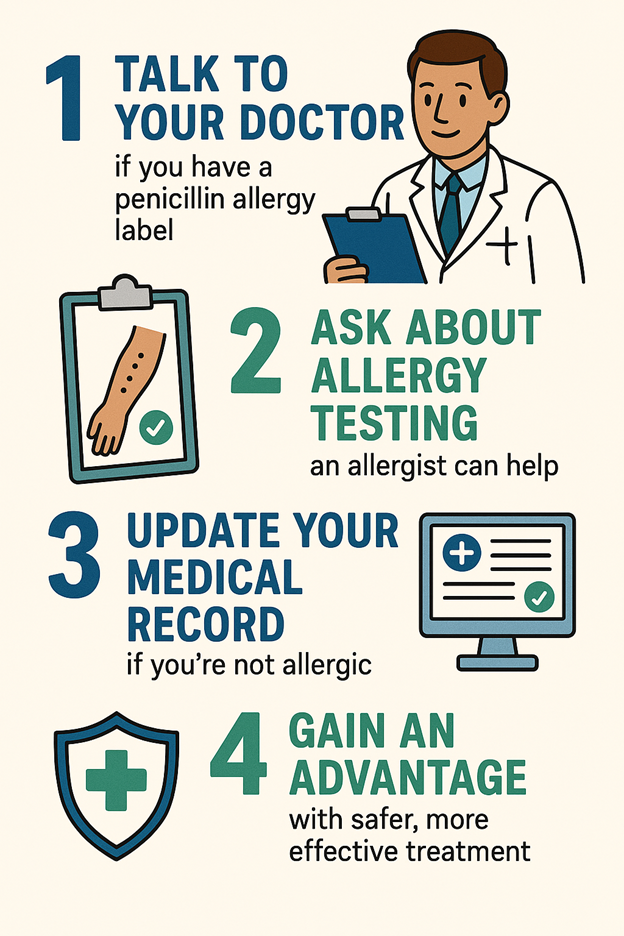
Talk to your doctor. If you were labeled allergic as a child or many years ago, it’s worth revisiting. Many allergy labels are based on outdated or unclear information and may no longer be accurate. Ask about allergy testing. A simple evaluation by an allergist, often including skin testing, can confirm whether you’re truly allergic. This helps avoid unnecessary use of less ideal or more powerful antibiotics.
If testing shows you’re not allergic, make sure your medical record is corrected. This can impact emergency care, antibiotic choices during hospitalizations or surgeries and result in safer and more effective treatment options in the future. Removing an incorrect allergy label can protect your health and help reduce antibiotic resistance for everyone.
Key Takeaway
Penicillin allergies are often misdiagnosed, outdated or no longer active. Talk to your doctor, get tested and update your records. Your future health may depend on it.
This article contains general information only and should not be used as a substitute for professional diagnosis, treatment or care by a qualified health care provider.