Summer is a great time to enjoy outdoor activities but it’s also in the middle of tick season, which can pose a danger to your health. Keystone Infectious Disease’s Medical Director, Dr. Raghavendra Tirupathi, and medical students studying under him, Rutvi Patel, Namrata Gajjala and Aparajitha Rajkumar answer common questions about Lyme disease and other tick-borne diseases in today’s Take Care article.
Summer is a great time to enjoy outdoor activities but it’s also in the middle of tick season, which can pose a danger to your health. Keystone Infectious Disease’s Medical Director, Dr. Raghavendra Tirupathi, and medical students studying under him, Rutvi Patel, Namrata Gajjala and Aparajitha Rajkumar answer common questions about Lyme disease and other tick-borne diseases in today’s Take Care article.
What Is Lyme Disease?
Lyme Disease is the most common tick-borne illness found in the United States and Europe. It is caused by a bacterium called Borrelia burgdorferi, which is transmitted through the bite of infected deer ticks, also known as blacklegged ticks.
Where Are the High-Risk Areas For Lyme Disease In The US?
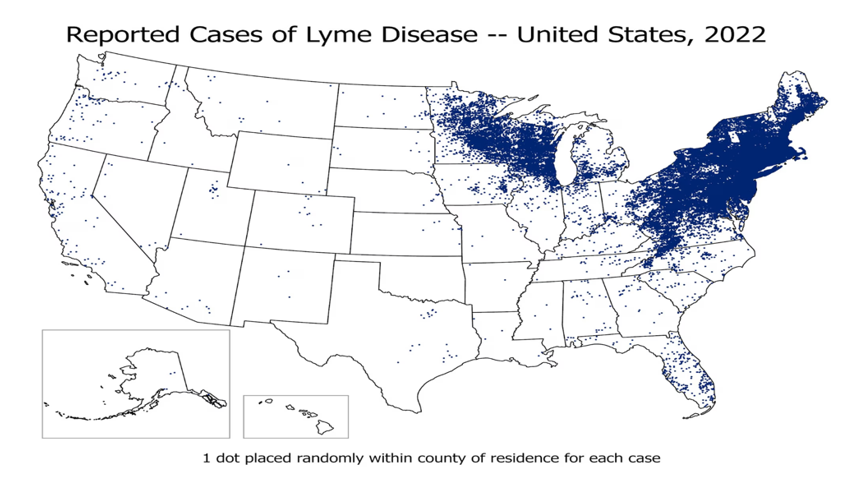
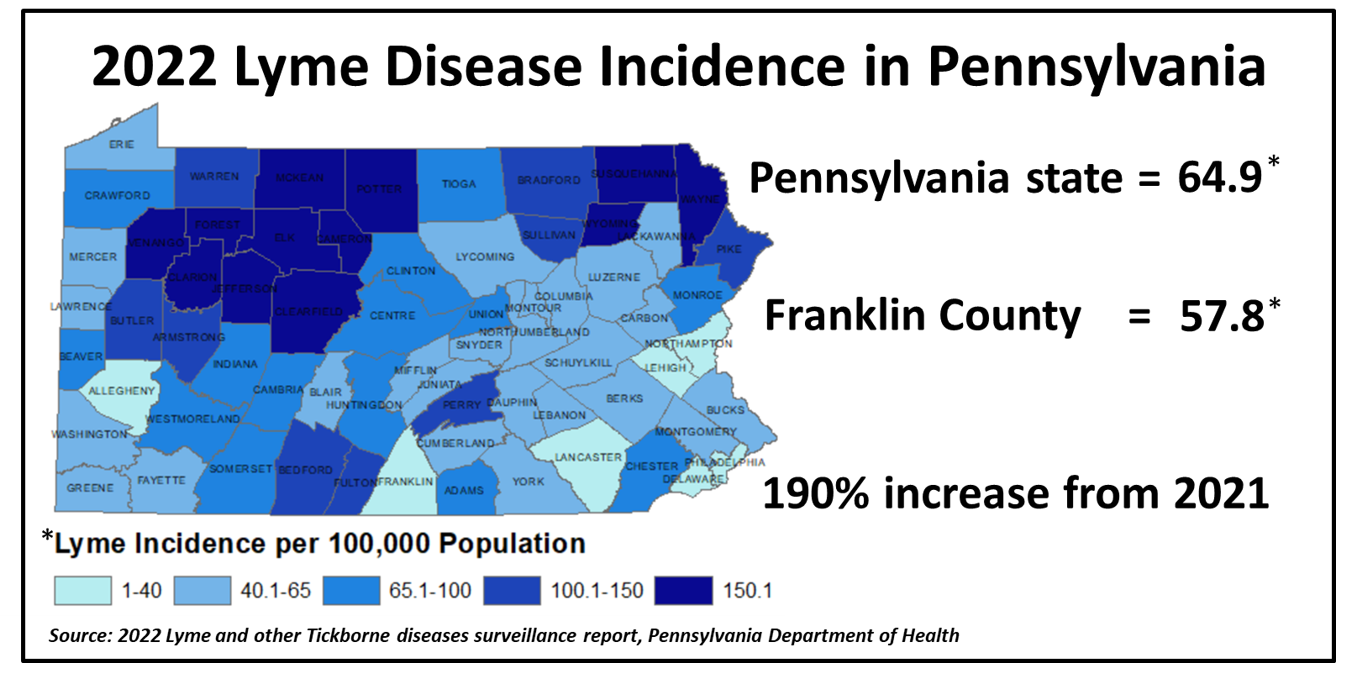
It is only possible to get Lyme disease from ticks which carry the bacteria. In high-risk areas, about 10–50% of deer ticks carry the bacteria. These include Eastern states, The Great Lakes Region, Northern Midwestern states and the West Coast. Each year, the Centers for Disease Control and Prevention (CDC) receives approximately 30,000 reports of Lyme disease from state health departments, but some data suggests as many as 476,000 people could have the disease each year. Pennsylvania leads the US in Lyme disease cases, with as many as 30% of all reported cases occurring in the state.
How Is Lyme Disease Transmitted?
Lyme disease is transmitted by deer tick bites, with the risk depending on geographic location, season, tick type and attachment duration. Ticks must be attached for more than 24 hours and need to feed for over 36 hours to become engorged with blood and capable of transmitting the disease. Moreover, the risk of transmission is higher after 72 hours. An unattached tick poses no risk of transmission. Lyme disease is not spread person-to-person through touching, kissing or sexual contact.
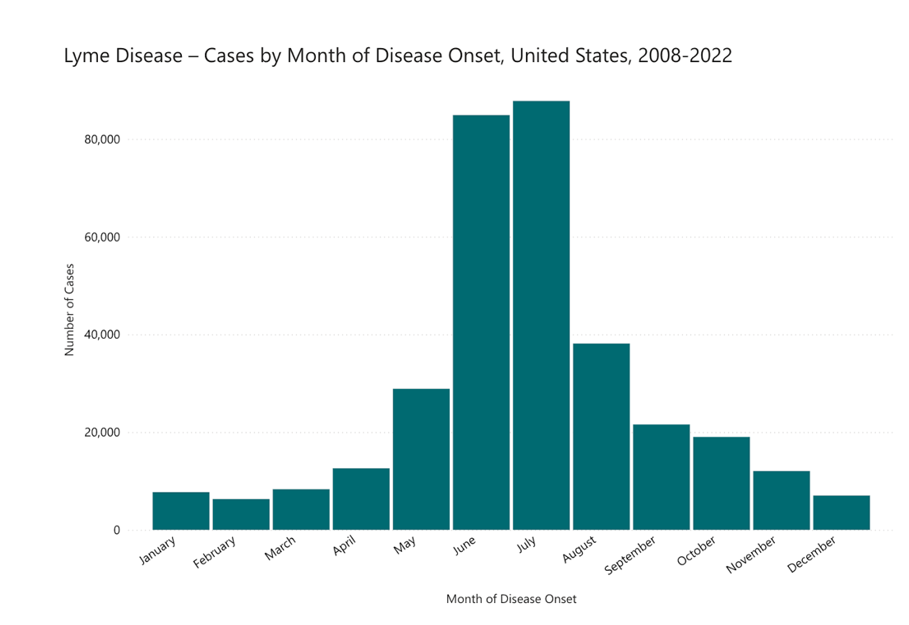
The risk of acquiring Lyme disease from a tick bite is 1-3% in prevalent areas and is more common during late spring and summer months, peaking in June and July. Prompt tick removal reduces this risk. As you can see below, tick bites are most common from April to September, peaking in June and July, but can happen all year round.
What Should I Do If I Get A Tick Bite?
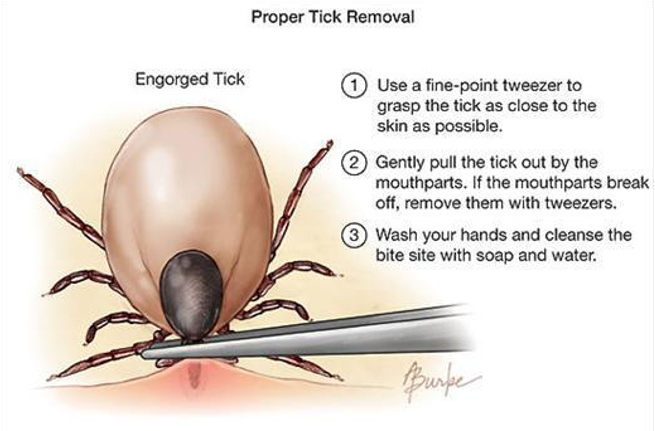
If you get a tick bite, it’s best to remove the tick as soon as possible using a three-step method. First, use curved tweezers to grasp the tick as close to the skin surface as possible. Avoid using a cigarette, petroleum jelly or liquid soap to remove the tick, as these substances may irritate the tick and cause it to behave like a syringe, injecting its bodily fluids into the wound. Next, pull the tweezers with the tick backward, gently and firmly. Do not jerk, twist, squeeze, crush or puncture the tick’s body, as its bodily fluids may contain infection-causing organisms.
If any mouth parts of the tick remain in the skin, leave them alone; they will be expelled naturally. Attempts to remove these parts may result in significant skin trauma. However, if more than half of the tick remains or if you’re unsuccessful in removing it, seek medical attention for expert removal.
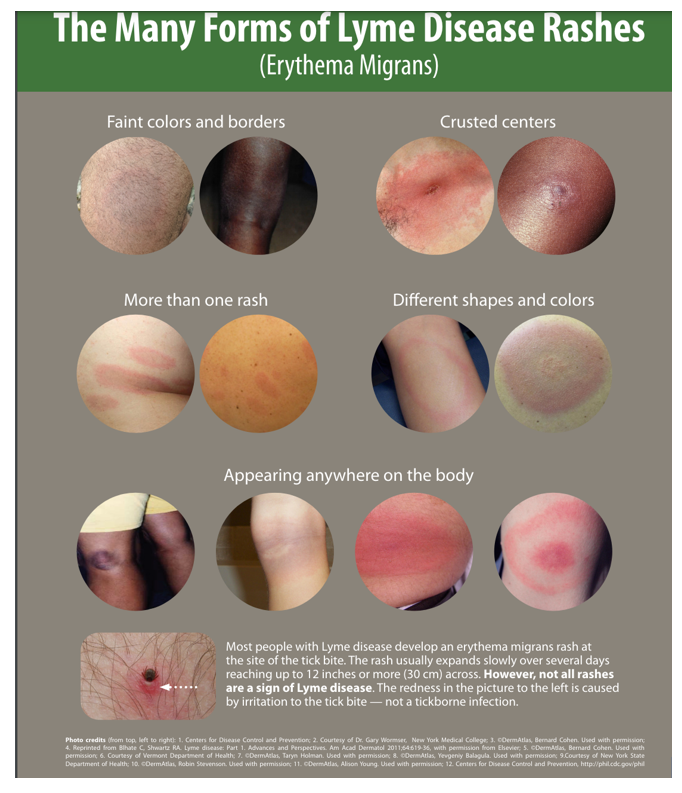
Lastly, after removing the tick, wash the skin and hands thoroughly with soap and water. It’s advisable to note the appearance of the tick, as only the deer tick can transmit Lyme disease. Observe the bite area for up to 30 days following the tick bite. Look for the development of a circular rash called a “bull’s-eye.” If a rash develops, contact your healthcare provider promptly.
What Are The Symptoms And When Should I Seek Medical Care?
If you experience any rash or flu-like symptoms such as fever, headache, fatigue or joint pain, it is best to seek healthcare advice. While a small bump at the bite site is typical, if the bite site becomes painful, swollen or oozing, it may indicate infection and require immediate attention. A rash that resembles a bull’s-eye, with central paleness and a circle of redness, is highly indicative of Lyme disease. Rarely, weakness and uncoordinated movement can accompany the rash, which is concerning.
How Is Lyme Disease Diagnosed?
Lyme disease is primarily diagnosed clinically. Specific signs, such as the characteristic rash, weakness or arthritis, along with a history of exposure to ticks or tick bites (especially the deer tick), can help narrow down the diagnosis of Lyme disease compared to other similar viral illnesses. However, a blood test can be used to check for Lyme disease antibodies, which may only test positive after 6 weeks. An early test is likely to be negative.
Should I Get The Tick Tested?
The CDC strongly discourages using tick test results to make decisions about antibiotics, as the results may not be reliable due to variations in quality standards across different laboratories. However, it is advisable to consult with your healthcare provider or a local lab for tick testing. The presence of germs in a tick does not necessarily indicate that the person is infected. Negative results can also be misleading, as another infected tick may have bitten the person unknowingly. Check out the Pennsylvania state DOH website for details about the tick testing laboratories.
Can Lyme Disease Be Treated?
Yes, Lyme disease is treated if symptoms develop and/or tests come back positive. Early diagnosis and treatment help prevent complications such as facial nerve palsy, meningitis, cardiac issues, chronic arthritis and progressive encephalomyelitis (inflammation of the brain and spinal cord). Oral antibiotics like doxycycline, amoxicillin or cefuroxime axetil are effective, while intravenous antibiotics are necessary for severe symptoms.
Can Lyme Disease Be Prevented?
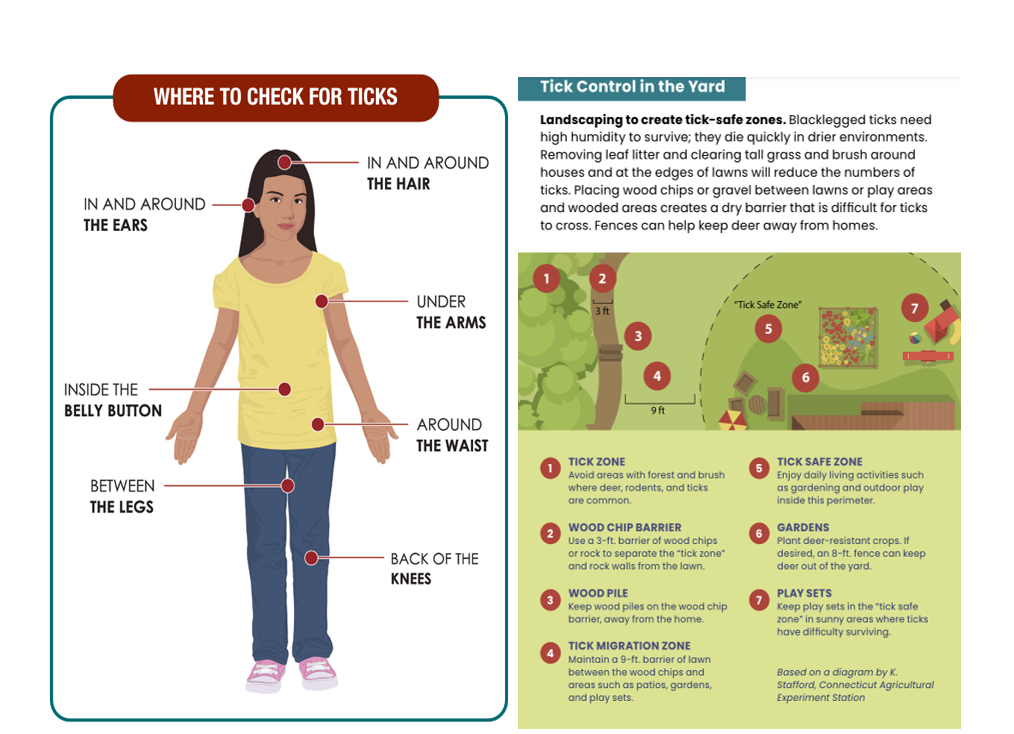
To prevent Lyme disease, avoiding tick bites is essential. Ticks are commonly found in grassy, brushy or wooded areas, so it’s best to steer clear of such environments. When spending time outdoors, sticking to the center of trails helps minimize contact with ticks. Caution should be exercised with pets and outdoor activities, as ticks can also be found on animals. Even in your own yard, steps should be taken to maintain a clean environment and reduce tick exposure.
After outdoor activities, check clothing for ticks before entering the home. Tumble-drying clothes on high heat for 10 minutes kills ticks on dry clothing. Showering with hot water within two hours of coming indoors reduces tick-borne disease risk and helps wash off unattached ticks. Conduct a full body check, including hard-to-reach areas, after returning from tick-infested areas. Check pets for ticks too; finding a crawling tick suggests others may be present.
Can I Use A Tick Repellent?
For effective tick repellent, consider using products containing active ingredients like DEET, picaridin or IR3535 (in 20% concentration). However, products with more than 50% DEET do not necessarily provide extra protection against tick bites. These repellents can be applied directly to the skin using creams, sprays or wipes. The United States Environmental Protection Agency website offers a helpful search tool to find the right product for your needs. Additionally, clothing, boots and camping gear can be treated with products containing 0.5% permethrin. Permethrin-treated items remain protective even after several washes. Alternatively, premade permethrin-treated clothing and gear are available.

Do I need Antibiotics Following A Tick Bite?
The CDC generally does not recommend antibiotics to prevent diseases after tick bites. However, preventive treatment with a single dose of doxycycline within 72 hours is recommended if the attached tick is identified as a deer tick, has been attached for 36 hours or more and the bite occurs in an area where deer ticks are common. Those who are pregnant or are less than 4 years old should not be treated with doxycycline.
Do Ticks Transmit Other Diseases?
Deer ticks can transmit multiple diseases alongside Lyme disease, resulting in co-infections. Anaplasmosis, caused by A. phagocytophilum bacteria, is spread by deer ticks and is the most common co-infection with Lyme disease. Symptoms include fever, headache, chills and muscle aches. Doxycycline serves as the standard treatment for both Lyme disease and anaplasmosis. Other co-infections, such as babesiosis, Powassan virus disease and hard tick relapsing fever, are less common but still significant.
By taking proper precautions and performing skin checks on yourself, children and pets after spending time outdoors, you can greatly reduce the chances of tick-borne illness.
This article contains general information only and should not be used as a substitute for professional diagnosis, treatment or care by a qualified health care provider.